PPPD and Vestibular Rehabilitation: What to Expect in Therapy
Persistent Postural-Perceptual Dizziness (PPPD) can be a challenging condition for those affected by it, often causing chronic dizziness, unsteadiness, and sensitivity to visual movement. However, for many with PPPD, vestibular rehabilitation therapy (VRT) offers a pathway toward improved balance, reduced dizziness, and better quality of life. In this post, we’ll dive into what PPPD is, how vestibular rehabilitation can help, and what to expect in therapy.
What is PPPD?
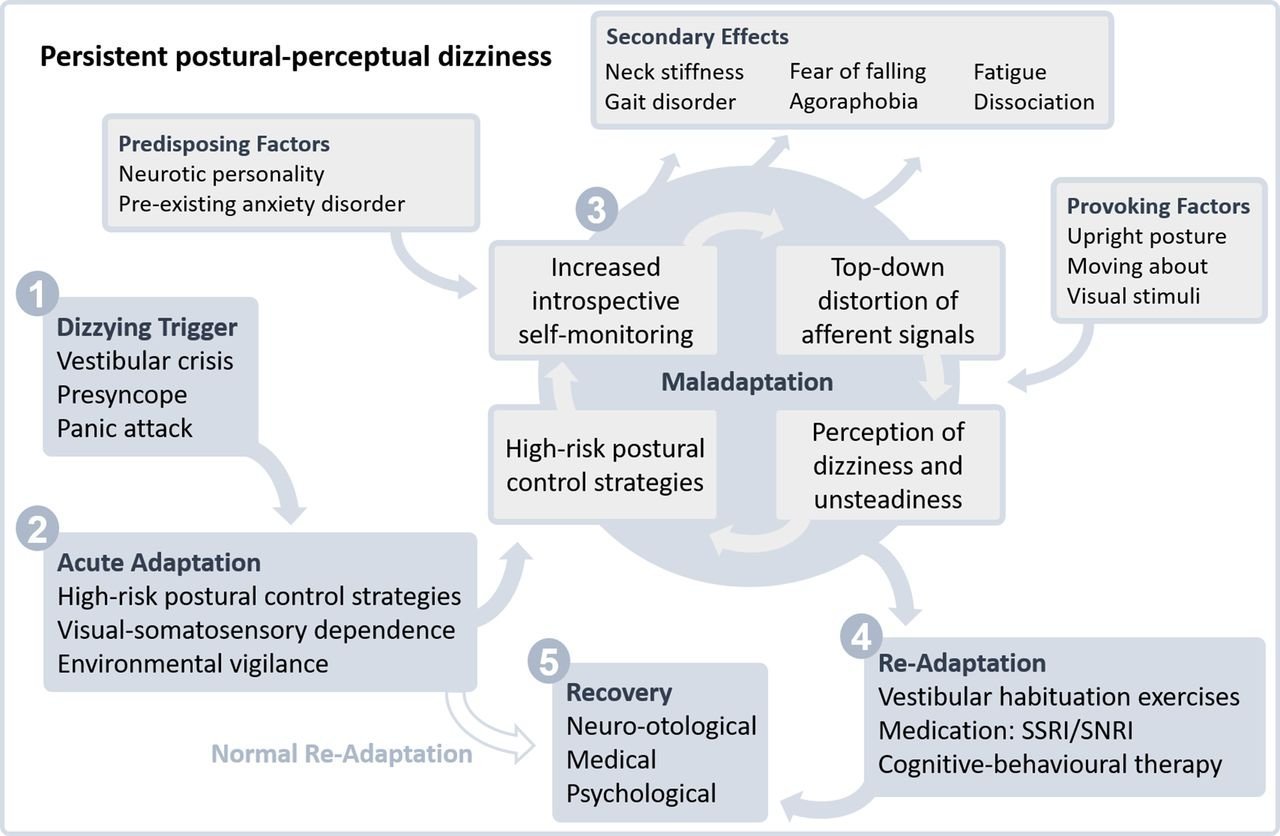
PPPD is a chronic disorder that affects balance and perception. People with PPPD often feel dizzy or unsteady even when they’re not moving, which can make activities like walking through busy places, driving, or even watching TV challenging. PPPD can result from an initial vestibular event, like vertigo or a balance disorder, and often continues beyond the resolution of the original condition. It’s believed that this condition involves an interaction between the brain’s perception of motion and balance and how it processes sensory information. PPPD is unique in that symptoms are often provoked by things that wouldn’t normally be problematic, such as crowded environments, fast-moving visuals, or even certain head movements.
How Can Vestibular Rehabilitation Help with PPPD?
Vestibular rehabilitation therapy (VRT) is a specialized form of physical therapy designed to help individuals improve balance and reduce dizziness through exercises that retrain the brain. With PPPD, VRT focuses on reducing symptom triggers, improving balance, and helping clients gradually become more comfortable with challenging movements or environments. By working on balance, coordination, and gradually reintroducing triggering movements, VRT can help the brain adapt and improve how it processes motion and sensory information.
What to Expect in Therapy
If you’re starting VRT for PPPD, here’s what you can generally expect in a typical treatment plan:
1. Initial Assessment
The first step of VRT is a thorough assessment. Your therapist will take a detailed history of your symptoms, triggers, and how PPPD affects your daily life. They may evaluate your balance, eye movements, and posture. This assessment helps create a tailored therapy plan to meet your unique needs and goals.
2. Setting Goals and Tracking Progress
Setting goals is a crucial part of VRT. Goals may include being able to walk confidently in a busy environment, sit comfortably in front of a screen, or even return to work. These benchmarks not only help guide therapy but also serve as motivation and measure progress over time.
3. Balance and Gaze Stabilization Exercises
Balance and gaze stabilization exercises are core elements of VRT. Balance training might include standing on different surfaces, performing activities that challenge coordination, or exercises on foam pads. Gaze stabilization exercises, on the other hand, help retrain the brain to control eye movements and improve visual stability. These exercises are often simple but require focus and consistency.
4. Exposure to Triggers in a Controlled Environment
Since PPPD symptoms are often triggered by certain movements or visual stimuli, part of VRT involves gradual exposure to these triggers in a controlled setting. Your therapist may use visual exercises or have you walk through specific movements that elicit symptoms. Gradually reintroducing these triggers helps the brain learn to process them more effectively and reduces the dizziness response over time.
5. Learning Breathing and Relaxation Techniques
Many people with PPPD also experience anxiety related to their symptoms, which can exacerbate dizziness and discomfort. In therapy, you might learn relaxation techniques such as deep breathing, mindfulness, and grounding exercises. These techniques can help manage anxiety, making it easier to focus on balance and movement tasks without stress.
6. Homework and Consistency
Like most physical therapy, VRT is most effective when exercises are practiced consistently outside of clinic visits. Your therapist will likely give you a set of home exercises designed to reinforce what you practice in sessions. Regular practice helps solidify improvements and trains the brain to adapt more quickly.
7. Tracking and Adjusting the Treatment Plan
As you progress, your therapist will work with you to track improvements and make adjustments as needed. Some exercises may become more challenging, while others may be modified based on what is most effective for you. The goal is to keep moving forward without overwhelming your system, creating gradual and sustained improvements.
Tips for Getting the Most Out of Vestibular Rehabilitation
Practice Patience: Adapting to new movements or stimuli can be challenging, and progress may seem slow at times. Remember that consistency is key.
Be Open with Your Therapist: Share any new symptoms or challenges you experience. Your therapist can adjust exercises and address concerns to make your sessions as effective as possible.
Practice Self-Care: Pay attention to things like hydration, nutrition, and sleep. Self-care supports your body’s healing process and helps keep dizziness at bay.
Set Small Milestones: Celebrating small wins—like feeling steadier on your feet or managing a busy environment—can boost confidence and help you stay motivated.
For those with PPPD, vestibular rehabilitation therapy offers a structured and supportive path to managing symptoms and reclaiming day-to-day activities. Through a tailored approach, VRT helps improve balance, reduce dizziness, and build confidence. Although progress may take time, with consistency, patience, and the right support, you can take significant steps toward a life with fewer PPPD symptoms.
If you’re interested in learning more about how vestibular rehabilitation can help with PPPD or would like to book an assessment, our clinic is here to guide you on your path to recovery!